A new study from the Hengen Lab published in Neuron takes a closer look how diseases like Alzheimer’s affect cell teamwork.
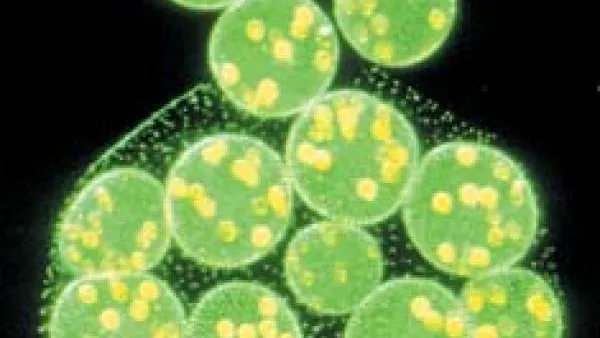
To function properly, our brains need to maintain balance—a homeostatic set-point called criticality. “It’s as excitable as the system can be without losing control,” Keith Hengen, Assistant Professor of Biology, explained. “At criticality, patterns of all sizes and time scales exist—as a result, a critical brain is optimal for computing almost anything.” So, if something upsets this balance, the brain’s ability to do things may start to unravel, like it does in diseases such as Alzheimer’s.
Hengen and his team looked at disease caused by a protein called tau that is involved in most forms of human neurodegeneration. In brains where everything is working properly, this protein helps stabilize structures inside neurons. But in neurodegenerative diseases, tau is assembled incorrectly and becomes toxic.
James McGregor, a postdoctoral researcher and first author, tracked the activity of neurons in the hippocampus of mice, looking for the ways in which tau changed things. Because neurodegenerative disease kills neurons, McGregor was surprised to find that the surviving individual neurons were working as expected—they fired at the same rate and variance as perfectly healthy neurons. However, when the team looked at what was happening on the slightly larger neural network-level, they found that, as a population, the neurons became worse at communicating as the disease progressed. Hengen compared this state to a dinner party gone awry: “If the individuals can’t speak, the conversation stops. That’s what we expected, but not what happened. Here, strangely enough, each friend is speaking normally, but the interactions between people are completely incoherent.”
Just like a dinner conversation can continue if one person leaves the table, it's well known that brains can compensate for the loss of many neurons—this is true in cases of both disease and injury. This study shows that the impact of neurodegenerative diseases like Alzheimer’s might be best explained by disruptions in how groups of neurons work together. “Without understanding how disease alters neuronal computation, we have no understanding of what the disease is, at a fundamental level,” Hengen said.
These changes in network function tracked with symptoms of the disease and could even predict the state of damage in the brain. Additionally, these shifts were dependent on whether the mouse was asleep or awake. “Based on other work from out lab, we think that a core function of sleep is to restore criticality in the brain,” Hengen said. In other words, sleep tries to restore criticality, but in disease, this doesn’t always work. “Our findings further push the idea that sleep and disease are two sides of the same coin.”
Looking toward the future, Hengen believes that these measures of dynamics and computational signatures could work as diagnostic tools. There is also further exploration to be done in the world of sleep and disease. McGregor said: “One of the exciting avenues that my work presents is the possibility of stopping or slowing disease by enhancing sleep. WashU is the best place in the world to be working on these problems.”